GM case-6
19. B.Namratha
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment"
A 38 year old man,who works as a chef hailing from Miryalaguda presented to the hospital with chief complaint of low fever since 10 days,abdominal pain,increased frequency of urination associated with pain and burning micturition since 1 week.
Date of admission:16-11-2021
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 1 week back.
C/o Low grade fever,intermittent associated with chills,headache(throbbing),nausea and body pains.Lower abdominal pain at umbilicus and groin pain were present.Not associated with cold and cough.
Burning micturition and increased frequency of urination(3 times in 30 mins).Urgency of urination was increased.Reddish colour urine with foul smell.
Routine:- He used to wake up at 8 A.M and have breakfast by 9 A.M and go to work by 10 A.M. Have lunch at work everyday by 2 P.M . Return home by 10 P.M have dinner and sleep by 12 A.M
PAST HISTORY:
There is no history of similar illness in the past.
The patient was diagnosed with Type II Diabetes Mellitus 3 years back and is on medication.He was on regular follow up.
No h/o Hypertension,CAD,Asthma,TB
No h/o surgeries in the past.
PERSONAL HISTORY:
The patient consumes mixed diet.
He appears to be adequately nourished.
Burning micturition.
Bowel movement is normal with dark brown coloured loose stools.
Appetite-Decreased
Sleep-Inadequate
The patient takes alcohol occasionally.
He smokes 2 cigarettes per day.
FAMILY HISTORY:
No history of similar complaints in the family.
TREATMENT HISTORY:
The patient is on medication for Type II Diabetes mellitus.
No drug allergies.
GENERAL EXAMINATION:
Patient was conscious, coherent and cooperative.well oriented to time place and person.
Built:well built
Nourishment: well nourished.
-No pallor
-No clubbing
-No cyanosis
-No icterus
-No generalized lymphadenopathy
-No pedal edema.
VITALS:
Vitals :
Temperature : Afebrile
Pulse rate: 86 beats per minute
Respiratory rate : 20 cycles per min
Bp :150/100mm of Hg.
SYSTEMIC EXAMINATION:
CVS:
S1 and S2 heard.
No cardiac murmurs.
RESPIRATORY SYSTEM:
Position of trachea- central
Normal vesicular breath sounds - heard
ABDOMEN:
Obese and soft abdomen.
Tenderness is present at the lower part of the abdomen.
Bowel sounds are heard.
CNS:
Patient is conscious.
Reflexes are normal
Speech is normal.
CLINICAL IMAGES:
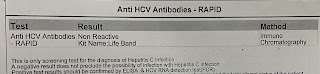
INVESTIGATIONS:
FEVER CHART:
PROVISIONAL DIAGNOSIS:
Acute pyelonephritis?Cystitis? k/c/o Type II DM
TREATMENT:
Inj.PIPTAZ 4.5gm IV/BD
Inj PAN 40mg/IV/OD
Inj ZOFER 4mg/IV/TID
Tab PCM 650 mg/PO/TID
Inj HAI s/c acc to GRBS
Inj OPHNEUM 1 amp in 100 ml.
Questions:
Why there is frequent urination?
Reason for the lower abdominal pain?



















Comments
Post a Comment