GM-Prefinals exam case
MEDICINE E-LOG BOOK
“This is an online e log book to discuss our patient’s de- identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence based inputs. This e-log book reflects my patient centered online portfolio and your valuable inputs on the comments is welcome.”
Date of admission:December 14,2021
36 YEAR OLD MAN WITH LOOSE STOOLS
-
A 36 year old man,who is a handloom weaver by occupation presented to the hospital with a chief complaint of loose stools since 4 to 5 months and generalised weakness since 4 to 5 months.
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 5 months back.Then he developed loose stools which lasted for 1 week and he went to a local hospital.After using the medication it got subsided.Then again when he stopped using the medication he developed loose stools again.The patient went to two to three local hospitals but the problem did not subside.
The patient used to pass stools after every meal(5-6 times per day).After passing stools the patient used to become weak.The patient complained to have a burning sensation while passing stools and that the stools had a foul smell and watery consistency.
No h/o blood in stools,fever,abdominal pain,vomitings.
The patient’s daily routine was to wake up at 5’o clock and have breakfast between 7 to 9 AM.Then he used to go to work i.e., weaving handlooms and used to come back and have lunch at 1pm. He used to take rest in the afternoons.He used to work again for some time and used to have dinner at 8pm and sleep at 9pm.
PAST HISTORY:
There is no history of similar illness in the past.
1 year back the patient had diminision of vision of both eyes and went to LV Prasad eye institute and was diagnosed with cataract.During the routine investigations it was found that he had high blood sugars and was started on OHAs.Then on follow ups the dose was escalated and finally switched to Injection mixtard and left eye cataract surgery was done.
No h/o Hypertension,Asthma,TB,CAD.
PERSONAL HISTORY:
The patient consumes mixed diet.
He appears lean and weak.
Appetite-normal
Sleep-Inadequate
Micturition-normal
Bowel movements-regular
The patient takes alcohol occasionally.
FAMILY HISTORY:
The patient’s mother is a k/c/o Diabetes.
TREATMENT HISTORY:
The patient is on Injection Mixtard 20U x 15U for diabetes.
No drug allergies.
GENERAL EXAMINATION:
Patient was conscious, coherent and cooperative.well oriented to time,place and person.
Built:The patient looks lean.
Nourishment: malnourished.
-No pallor
-No clubbing
-No cyanosis
-No icterus
-No generalized lymphadenopathy
-No pedal edema.
VITALS:
Temperature : Afebrile
Pulse rate: 80 beats per minute
Respiratory rate : 20 cycles per min
Bp :110/80mm of Hg.
SYSTEMIC EXAMINATION:
CVS:
S1 and S2 heard.
No cardiac murmurs.
RESPIRATORY SYSTEM:
Position of trachea- central
Normal vesicular breath sounds - heard
ABDOMEN:
Abdomen-Soft
No tenderness of abdomen.
Bowel sounds are heard.
CNS:
Patient is conscious.
Reflexes are normal
Speech is normal.
CLINICAL IMAGES:
INVESTIGATIONS:
FEVER CHART:
HIV TEST:GLUCOSE TOLERANCE TEST:
BLOOD SUGAR FASTING:
CBP:
ANTI HCV ANTIBODIES-RAPID:HBsAg-RAPID:
BACTERIAL CULTURE&SENSITIVITY REPORT:
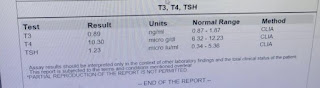
T3,T4,TSH:
SERUM CREATININE:
ULTRASOUND:
PROVISIONAL DIAGNOSIS:
- Osmotic diarrhea under evaluation
Secondary to
? Uncontrolled sugars
- ? Diabetic autonomic neuropathy
- Proteinuria under evaluation
- K/C/O DM
TREATMENT:
1.IVF -NS RL @75ml/hr
2.Inj.OPTINEURON 1amp in 100ml NS/IV/OF
3.Tab. PAN 40mg/PO/OD
4.Inj. H.mixtard s/c b
5.Tab. VILDAGLIPTIN 50mg/PO/OD
6.Tab. REDOTIL 100mg/PO/OD
7.Monitor vitals 4th hourly
8.Tab.SPOROLAC -DS /TID
9.Tab.Loperamide 2mg/PO/BD
10.ORS sachets 1sachet in 1L water; 200ml after each stool passed.





















Comments
Post a Comment